Search
- Page Path
- HOME > Search
- Miscellaneous
- Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
- Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon, Hwa Young Ahn, Hoon Sung Choi, Sang Mo Hong, Dong Yeob Shin, Ji A Seo, Se Hwa Kim, Seungjoon Oh, Sung Hoon Yu, Byung Joon Kim, Choong Ho Shin, Sung-Woon Kim, Chong Hwa Kim, Eun Jig Lee
- Endocrinol Metab. 2020;35(2):272-287. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.272
- 9,478 View
- 428 Download
- 13 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
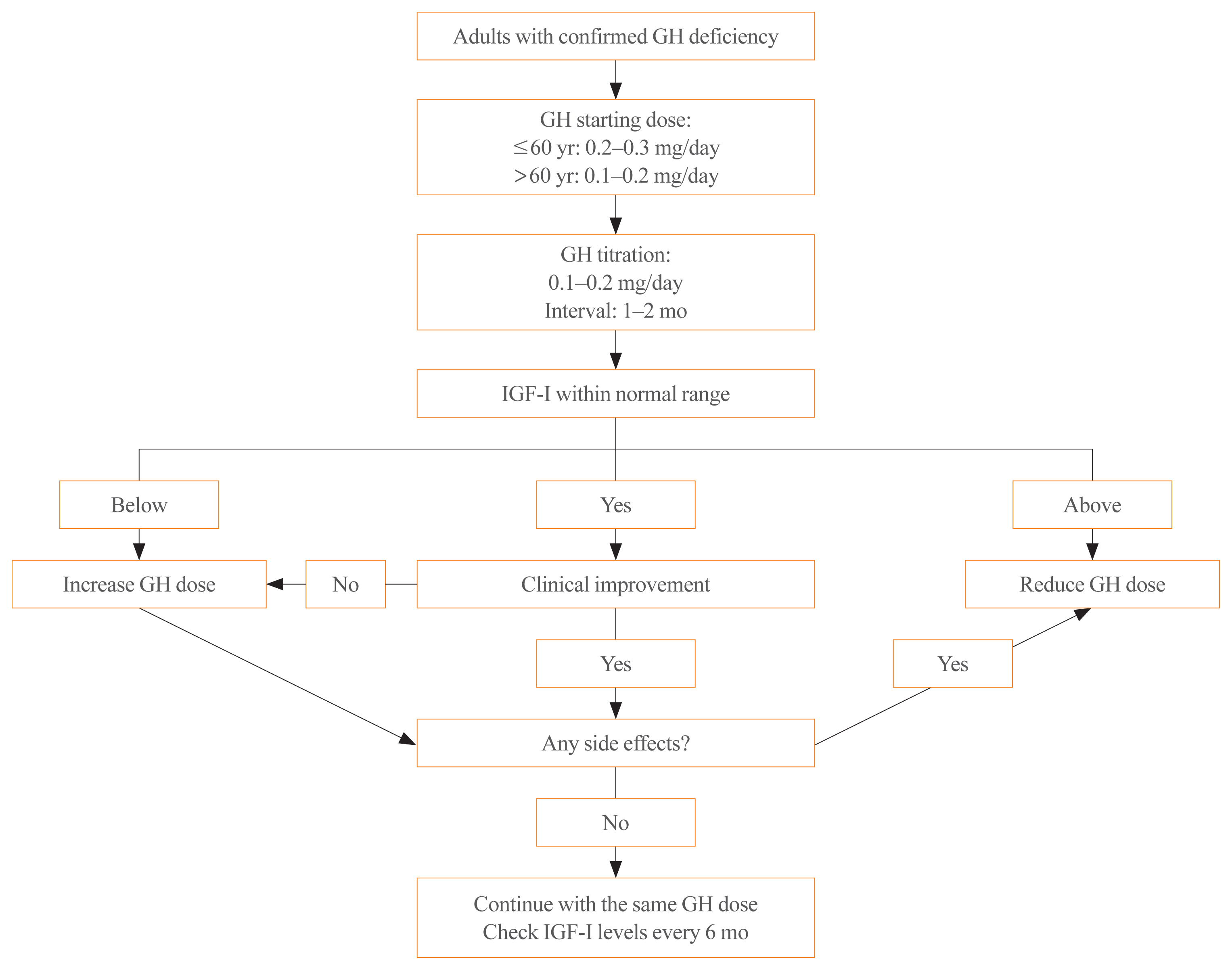
ePub - Growth hormone (GH) deficiency is caused by congenital or acquired causes and occurs in childhood or adulthood. GH replacement therapy brings benefits to body composition, exercise capacity, skeletal health, cardiovascular outcomes, and quality of life. Before initiating GH replacement, GH deficiency should be confirmed through proper stimulation tests, and in cases with proven genetic causes or structural lesions, repeated GH stimulation testing is not necessary. The dosing regimen of GH replacement therapy should be individualized, with the goal of minimizing side effects and maximizing clinical improvements. The Korean Endocrine Society and the Korean Society of Pediatric Endocrinology have developed a position statement on the diagnosis and treatment of GH deficiency. This position statement is based on a systematic review of evidence and expert opinions.
-
Citations
Citations to this article as recorded by- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Ghina Tsurayya, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, Muhammad Iqhrammullah
Children.2024; 11(2): 227. CrossRef - Evaluation of Adult Height in Patients with Non-Permanent Idiopathic GH Deficiency
Agnese Murianni, Anna Lussu, Chiara Guzzetti, Anastasia Ibba, Letizia Casula, Mariacarolina Salerno, Marco Cappa, Sandro Loche
Endocrines.2023; 4(1): 169. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Continuous Glucose Monitoring: A Possible Aid for Detecting Hypoglycemic Events during Insulin Tolerance Tests
Soo Yeun Sim, Moon Bae Ahn
Sensors.2023; 23(15): 6892. CrossRef - The risk patients with AGHD have of developing CVD
Eisha Javed, Maha Zehra, Naz Elahi
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 19: 200221. CrossRef - Diagnosis of GH Deficiency Without GH Stimulation Tests
Anastasia Ibba, Sandro Loche
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
Endocrinology and Metabolism.2022; 37(2): 359. CrossRef - A Radiomics-Based Model with the Potential to Differentiate Growth Hormone Deficiency and Idiopathic Short Stature on Sella MRI
Taeyoun Lee, Kyungchul Song, Beomseok Sohn, Jihwan Eom, Sung Soo Ahn, Ho-Seong Kim, Seung-Koo Lee
Yonsei Medical Journal.2022; 63(9): 856. CrossRef - Phenotypic spectrum of patients with mutations in CHD7: clinical implications of endocrinological findings
Ja Hye Kim, Yunha Choi, Soojin Hwang, Gu-Hwan Kim, Han-Wook Yoo, Jin-Ho Choi
Endocrine Connections.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Laron syndrome: clinic, diagnostics (а clinical case)
P.M. Lіashuk, R.P. Lіashuk, N.I. Stankova, M.B. Kudina
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 193. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - Asian Conference on Tumor Ablation guidelines for renal cell carcinoma
Byung Kwan Park, Shu-Huei Shen, Masashi Fujimori, Yi Wang
Investigative and Clinical Urology.2021; 62(4): 378. CrossRef - Diagnosis and Treatment of Adult Growth Hormone Deficiency
Jung Hee Kim
The Korean Journal of Medicine.2021; 96(5): 400. CrossRef
- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial

- Hypothalamus and Pituitary gland
- Medical Treatment with Somatostatin Analogues in Acromegaly: Position Statement
- Sang Ouk Chin, Cheol Ryong Ku, Byung Joon Kim, Sung-Woon Kim, Kyeong Hye Park, Kee Ho Song, Seungjoon Oh, Hyun Koo Yoon, Eun Jig Lee, Jung Min Lee, Jung Soo Lim, Jung Hee Kim, Kwang Joon Kim, Heung Yong Jin, Dae Jung Kim, Kyung Ae Lee, Seong-Su Moon, Dong Jun Lim, Dong Yeob Shin, Se Hwa Kim, Min Jeong Kwon, Ha Young Kim, Jin Hwa Kim, Dong Sun Kim, Chong Hwa Kim
- Endocrinol Metab. 2019;34(1):53-62. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.53
- 6,451 View
- 253 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub The Korean Endocrine Society (KES) published clinical practice guidelines for the treatment of acromegaly in 2011. Since then, the number of acromegaly cases, publications on studies addressing medical treatment of acromegaly, and demands for improvements in insurance coverage have been dramatically increasing. In 2017, the KES Committee of Health Insurance decided to publish a position statement regarding the use of somatostatin analogues in acromegaly. Accordingly, consensus opinions for the position statement were collected after intensive review of the relevant literature and discussions among experts affiliated with the KES, and the Korean Neuroendocrine Study Group. This position statement includes the characteristics, indications, dose, interval (including extended dose interval in case of lanreotide autogel), switching and preoperative use of somatostatin analogues in medical treatment of acromegaly. The recommended approach is based on the expert opinions in case of insufficient clinical evidence, and where discrepancies among the expert opinions were found, the experts voted to determine the recommended approach.
-
Citations
Citations to this article as recorded by- Hydrogel-fiber-mesh-based 3D cell cultures: A new method for studying pituitary tumors
Wooju Jeong, Sungrok Wang, Yumin Kim, Soohyun Lee, Minhu Huang, Jaeil Park, Myung-Han Yoon, Chang-Myung Oh, Cheol Ryong Ku
Smart Materials in Medicine.2024;[Epub] CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
A Ram Hong, Ho-Cheol Kang
Endocrinology and Metabolism.2023; 38(2): 175. CrossRef - Growth Hormone Excess: Implications and Management
Suneela Dhaneshwar, Shrishti Shandily, Vatsalya Tiwari
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(6): 748. CrossRef - Revisiting the usefulness of the short acute octreotide test to predict treatment outcomes in acromegaly
Montserrat Marques-Pamies, Joan Gil, Elena Valassi, Marta Hernández, Betina Biagetti, Olga Giménez-Palop, Silvia Martínez, Cristina Carrato, Laura Pons, Rocío Villar-Taibo, Marta Araujo-Castro, Concepción Blanco, Inmaculada Simón, Andreu Simó-Servat, Gemm
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Octreotide in the treatment of acromegaly – the possibilities of high-dose therapy
I. A. Ilovayskaya
Meditsinskiy sovet = Medical Council.2022; (10): 148. CrossRef - Approach of Acromegaly during Pregnancy
Alexandru Dan Popescu, Mara Carsote, Ana Valea, Andreea Gabriela Nicola, Ionela Teodora Dascălu, Tiberiu Tircă, Jaqueline Abdul-Razzak, Mihaela Jana Țuculină
Diagnostics.2022; 12(11): 2669. CrossRef - Left to themselves: Time to target chronic pain in childhood rare diseases
Christine B. Sieberg, Alyssa Lebel, Erin Silliman, Scott Holmes, David Borsook, Igor Elman
Neuroscience & Biobehavioral Reviews.2021; 126: 276. CrossRef - Severe respiratory failure in a patient with COVID-19 and acromegaly: rapid improvement after adding octreotide
Jacob Luty, LesleAnn Hayward, Melanie Jackson, P Barton Duell
BMJ Case Reports.2021; 14(8): e243900. CrossRef - Precision Therapy in Acromegaly Caused by Pituitary Tumors: How Close Is It to Reality?
Cheol Ryong Ku, Vladimir Melnikov, Zhaoyun Zhang, Eun Jig Lee
Endocrinology and Metabolism.2020; 35(2): 206. CrossRef - Medical Treatment with Somatostatin Analogues in Acromegaly: Position Statement
Sang Ouk Chin, Cheol Ryong Ku, Byung Joon Kim, Sung-Woon Kim, Kyeong Hye Park, Kee Ho Song, Seungjoon Oh, Hyun Koo Yoon, Eun Jig Lee, Jung Min Lee, Jung Soo Lim, Jung Hee Kim, Kwang Joon Kim, Heung Yong Jin, Dae Jung Kim, Kyung Ae Lee, Seong-Su Moon, Dong
The Korean Journal of Medicine.2019; 94(6): 485. CrossRef
- Hydrogel-fiber-mesh-based 3D cell cultures: A new method for studying pituitary tumors

- Adrenal gland
- Clinical Guidelines for the Diagnosis and Treatment of Cushing's Disease in Korea
- Kyu Yeon Hur, Jung Hee Kim, Byung Joon Kim, Min-Seon Kim, Eun Jig Lee, Sung-Woon Kim
- Endocrinol Metab. 2015;30(1):7-18. Published online March 27, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.1.7
- 6,694 View
- 151 Download
- 10 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Cushing's disease (CD) is a rare disorder characterized by the overproduction of adrenocorticotropic hormone due to a pituitary adenoma that ultimately stimulates excessive cortisol secretion from the adrenal glands. Prior to the detection of pituitary adenomas, various clinical signs of CD such as central obesity, moon face, hirsutism, and facial plethora are usually already present. Uncontrolled hypercortisolism is associated with metabolic, cardiovascular, and psychological disorders that result in increased mortality. Hence, the early detection and treatment of CD are not only important but mandatory. Because its clinical manifestations vary from patient to patient and are common in other obesity-related conditions, the precise diagnosis of CD can be problematic. Thus, the present set of guidelines was compiled by Korean experts in this field to assist clinicians with the screening, diagnoses, and treatment of patients with CD using currently available tests and treatment modalities.
-
Citations
Citations to this article as recorded by- Diet quality and dietary acid load in relation to cardiovascular disease mortality: Results from Fasa PERSIAN cohort study
Sahar Fereidouni, Najmeh Hejazi, Reza Homayounfar, Mojtaba Farjam
Food Science & Nutrition.2023; 11(3): 1563. CrossRef - Role of computed tomography in predicting adrenal adenomas with cortisol hypersecretion
Chan Kyo Kim, Kyung A Kang, Young Lyun Oh, Sung Yoon Park
The British Journal of Radiology.2023;[Epub] CrossRef - Dietary acid load and mortality from all causes, CVD and cancer: results from the Golestan Cohort Study
Ehsan Hejazi, Hadi Emamat, Maryam Sharafkhah, Atoosa Saidpour, Hossein Poustchi, Sadaf Sepanlou, Masoud Sotoudeh, Sanford Dawsey, Paolo Boffetta, Christian C Abnet, Farin Kamangar, Arash Etemadi, Akram Pourshams, Akbar Fazeltabar Malekshah, Paul Berennan,
British Journal of Nutrition.2022; 128(2): 237. CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - Pituitary adenomas: current principles of diagnosis and treatment
L. I. Astafyeva, I. V. Chernov, I. V. Chekhonin, E. I. Shults, I. N. Pronin, P. L. Kalinin
Russian journal of neurosurgery.2021; 22(4): 94. CrossRef - Metabolic changes in serum steroids for diagnosing and subtyping Cushing’s syndrome
Chang Ho Ahn, Chaelin Lee, Jaeyoon Shim, Sung Hye Kong, Su-jin Kim, Yong Hwy Kim, Kyu Eun Lee, Chan Soo Shin, Jung Hee Kim, Man Ho Choi
The Journal of Steroid Biochemistry and Molecular Biology.2021; 210: 105856. CrossRef - Application of different variants of endoscopic transphenoidal removal of corticotropinomas in order to increase the frequency and duration of remission
A. Ashraf, I. V. Chernov, A. N. Shkarubo, M. A. Kutin, D. V. Fomichev, O. I. Sharipov, Yu. Yu. Trunin, D. N. Andreev, A. A. Abdilatipov, L. I. Astafieva, B. Abdali, A. B. Kurnosov, G. E. Chmutin, Kalinin P. L. Kalinin P. L.
Vestnik nevrologii, psihiatrii i nejrohirurgii (Bulletin of Neurology, Psychiatry and Neurosurgery).2021; (2): 143. CrossRef - Modern aspects of surgery for cushing’s disease
A. Abdali, L.I. Astafeva, Yu.Yu. Trunin, I.V. Chernov, Yu.G. Sidneva, A.A. Abdilatipov, P.L. Kalinin
Voprosy neirokhirurgii imeni N.N. Burdenko.2021; 85(4): 111. CrossRef - Pituitary microadenomas — current diagnostic and treatment methods
L.I. Astafyeva, B.A. Kadashev, Yu.G. Sidneva, I.V. Chernov, P.L. Kalinin
Voprosy neirokhirurgii imeni N.N. Burdenko.2020; 84(2): 110. CrossRef - Usefulness of prolactin measurement in inferior petrosal sinus sampling with desmopressin for Cushing’s syndrome
Hamideh Akbari, Mohammad Ghorbani, Maryam Kabootari, Ali Zare Mehrjardi, Mohammad Reza Mohajeri Tehrani, Mojtaba Malek, Mohammad E. Khamseh
British Journal of Neurosurgery.2020; 34(3): 253. CrossRef - Hormonal aggressiveness according to the expression of cellular markers in corticotroph adenomas
Jung Soo Lim, Mi-Kyung Lee, Eunhee Choi, Namki Hong, Soo Il Jee, Sun Ho Kim, Eun Jig Lee
Endocrine.2019; 64(1): 147. CrossRef - Clinical Parameters to Distinguish Silent Corticotroph Adenomas from Other Nonfunctioning Pituitary Adenomas
Daham Kim, Cheol Ryong Ku, Se Hee Park, Ju Hyung Moon, Eui Hyun Kim, Sun Ho Kim, Eun Jig Lee
World Neurosurgery.2018; 115: e464. CrossRef - Blood Tests for the Diagnosis of Adrenal Diseases
Seon-Ah Cha, Sung-Dae Moon
The Korean Journal of Medicine.2018; 93(6): 532. CrossRef - Choosing wisely: la lista del gruppo di studio Endocrinologia e Malattie del Metabolismo della Società Italiana di Patologia Clinica e Medicina di Laboratorio
Romolo M. Dorizzi, Anna Ferrari, Marina Vitillo, Beatrice Caruso, Claudio Cocco, Erennio Ciotoli, Federica D’Aurizio, Elisa Esposito, Germana Giannone, Giulio Ozzola, Ottavia Porzio, Emanuela Toffalori, Renato Tozzoli
La Rivista Italiana della Medicina di Laboratorio - Italian Journal of Laboratory Medicine.2016; 12(2): 81. CrossRef - Surgical management of adrenocorticotropic hormone-secreting pituitary adenomas
Edwin S Kulubya, Daniel A Donoho, John D Carmichael, Gabriel Zada
International Journal of Endocrine Oncology.2016; 3(1): 41. CrossRef
- Diet quality and dietary acid load in relation to cardiovascular disease mortality: Results from Fasa PERSIAN cohort study

- A Case of Adrenal Teratoma.
- Ji young Kim, Youn zoo Cho, Kang Woo Lee, Dong Mee Lim, Keun Young Park, Byung Joon Kim
- Endocrinol Metab. 2011;26(3):272-275. Published online September 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.3.272
- 65,956 View
- 21 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Teratoma is a congenital tumor containing tissues derived from all germ layers. Teratoma in the region of the adrenal gland is a very uncommon retroperitoneal tumor. Only 7 cases of adrenal teratoma have been reported worldwide, but in Korea, no similar cases have been reported until now. This case report describes an adrenal teratoma in a 38-year-old healthy woman who was incidentally diagnosed with a left adrenal mass on abdominal ultrasonography during a medical inspection. Computed tomographic scans revealed a 9-cm heterogeneous circumscribed round mass, containing primarily fat tissue, and a solid calcification component in the left adrenal gland. Adrenal hormonal assessment results and biochemical markers for gonadal neoplasia were negative. Result of serum laboratory tests were normal. The patient underwent laparoscopic adrenalectomy. Histologic analysis confirmed the diagnosis of a mature teratoma; the obtained specimen measured 5 x 7 x 7.5 cm and weighed 267 g. The surface of the mass was smooth, and sebaceous tissue and hair with hard material were observed on the incisional surface. The patient was discharged on postoperative day 4, without complications. In this case report, we describe the incidental finding of a teratoma occurring in the adrenal gland region in a healthy woman; the teratoma was laparoscopically excised.
-
Citations
Citations to this article as recorded by- Lipomatous tumours in adrenal gland: WHO updates and clinical implications
Alfred King-yin Lam
Endocrine-Related Cancer.2017; 24(3): R65. CrossRef - A Case of Teratoma of Thyroid Gland in Adolescence
Yu-Chang Lee, Su-Jin Jeong, Sol-Jae Lee, Chong-Hwa Kim, Yong-Hoon Lee, Jung-Eun Lee, Hye-Ji Seo
International Journal of Thyroidology.2017; 10(1): 61. CrossRef
- Lipomatous tumours in adrenal gland: WHO updates and clinical implications

- GLP-1 Can Protect Proinflammatory Cytokines Induced Beta Cell Apoptosis through the Ubiquitination.
- Dong Mee Lim, Ju Young Kim, Kang Woo Lee, Keun Young Park, Byung Joon Kim
- Endocrinol Metab. 2011;26(2):142-149. Published online June 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.2.142
- 1,617 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Proinflammatory cytokines are one of the causes of diabetes mellitus. However, the exact molecular mechanism by which proinflammatory cytokines induce beta-cell death remains to be clearly elucidated. Glucagon-like peptide-1 (GLP-1) affects the stimulation of insulin secretion and the preservation of beta-cells. Additionally, it may exert an antiapoptotic effect on beta cells; however, the mechanism underlying this effect has yet to be demonstrated. Therefore, we investigated the protective effects of GLP-1 in endoplasmic reticulum (ER)-mediated beta-cell apoptosis using proinflammatory cytokines. METHODS: To induce ER stress, hamster insulin-secreting tumor (HIT)-T15 cells were treated using a mixture of cytokines. Apoptosis was evaluated via MTT assay, Hoechst 33342 staining, and annexin/propidium iodide (PI) flow cytometry. The mRNA and protein expression levels of ER stress-related molecules were determined via PCR and Western blotting, respectively. Nitric oxide was measured with Griess reagent. The levels of inducible nitric oxide synthase (iNOS) mRNA and protein were analyzed via real-time PCR and Western blot, respectively. iNOS protein degradation was evaluated via immunoprecipitation. We pretreated HIT-T15 cells with exendin (Ex)-4 for 1 hour prior to the induction of stress. RESULTS: We determined that Ex-4 exerted a protective effect through nitric oxide and the modulation of ER stress-related molecules (glucose-regulated protein [GRP]78, GRP94, and CCAAT/enhancer-binding protein homologous protein [CHOP]) and that Ex-4 stimulates iNOS protein degradation via the ubiquitination pathway. Additionally, Ex-4 also induced the recovery of insulin2 mRNA expression in beta cells. CONCLUSION: The results of this study indicate that GLP-1 may protect beta cells against apoptosis through the ubiquitination pathway.

- A Case of Coexistence of Parathyroid and Papillary Thyroid Carcinoma.
- Yoon Shick Yom, Myung Jun Lee, Hyun Woo Lim, Jeong Ho Park, Sung Tae Kim, Yu Mi Lee, Dong Ju Yang, Youn Zoo Cho, Moon Il Park, Kang Woo Lee, Keun Young Park, Dong Mee Lim, Byung Joon Kim
- J Korean Endocr Soc. 2010;25(1):61-67. Published online March 1, 2010
- DOI: https://doi.org/10.3803/jkes.2010.25.1.61
- 1,654 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Primary hyperparathyroidism is usually caused by a parathyroid adenoma, occasionally by primary parathyroid hyperplasia and rarely by parathyroid carcinoma. Coincidental occurrence of thyroid carcinoma in parathyroid adenoma is not uncommon, but synchronous parathyroid and thyroid carcinoma is extremely rare. Here, we describe a case of synchronous parathyroid carcinoma and papillary thyroid carcinoma.

- A Case of Prolonged Hypoglycemia Post Topiramate Treatment an Anti-convulsant, in a Type 2 Diabetic Patient.
- Myung Jun Lee, Yoon Shick Yom, Hyun woo Lim, Sung Tae Kim, Yu Mi Lee, Youn Zoo Cho, Kang Woo Lee, Byung Joon Kim, Keun Young Park, Dong Mee Lim
- J Korean Endocr Soc. 2009;24(4):277-280. Published online December 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.4.277
- 3,711 View
- 92 Download
-
 Abstract
Abstract
 PDF
PDF - Topiramate is a drug used to treat epilepsy, and is known for its effects including reduced appetite resulting in lower body weight, and the lowering of neutral fat. In addition, topiramate is known to reduce blood sugar levels by increasing insulin sensitivity and by increasing insulin secretion by glucose stimulation. The authors report a case of persistent hypoglycemia, in a patient who had been administrating topiramate, as a treatment for epilepsy following an episode of cerebral infarction.

- Cholesterol Lowering Effect of Cerivastatin in Korean Patients with Primary Hypercholesterolemia.
- Sung Hoon Kim, Dong Jun Kim, Jong Rhulk Hahm, Byung Joon Kim, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim
- J Korean Endocr Soc. 1999;14(4):729-738. Published online January 1, 2001
- 1,243 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cerivastatin is a kind of statin, a synthetic HMG-CoA reductase inhibitor with high liver selectivity which lowers plasma cholesterol level by inhibiting endogenous cholesterol synthesis. This study evaluates the efficacy, safety, and tolerability of cerivastatin 0.1 mg and 0.3 mg in Korean patients with primary hypercholesterolemia. METHODS: A parallel group, randomized, placebo-controlled, double-blind study was conducted at Samsung Medical Center. The patients with primary hypercholesterolemia were placed on an American Heart Association Step 1 diet for whole study period. Single-blind placebo was administered for the final 4 weeks of period A, before randomization. Thirty two patients with low-density lipoprotein cholesterol (LDL-C) >160 mg/dL (if patients with a definite personal history of coronary heart disease (CHD) or with two or more cardiovascular risk factors, LDL-C >130 mg/dL) were randomized to 6 weeks treatment with one of the following regimens: cerivastatin 0.1 mg (n=11) or cerivastatin 0.3 mg (n=10) or placebo once daily at bedtime (n=11). RESULTS: Cerivastatin 0.1 mg and 0.3 mg treatment groups produced statistically significant (p<.05) changes at 6 weeks after treatment, compared to baseline and placebo in LDL-C (cerivastatin 0.1 mg 16.3%; cerivastatin 0.3 mg 35.2%; placebo 1.5%) and total cholesterol (cerivastatin 0.1 mg 10.3%; cerivastatin 0.3 mg 26.2%; placebo 1.3%). Cerivastatin 0.1 mg and 0.3 mg treatments were well tolerated and resulted in no significant increase in biochemical or clinical side effects compared to placebo. CONCLUSION: Cerivastatin at doses of 0.1 mg and 0.3 mg/day is a safe, well-tolerated, and highly effective HMG-CoA reductase inhibitor for the treatment of primary hypercholesterolemia.

- ret/PTC-1, -2, and -3 Incogene Rearrangements of Papillary Thyroid Carcinomas in Korea and Its Relevance to Clinical Aggressiveness.
- Jong Ryeal Hanhm, Jae Hoon Chung, Byung Joon Kim, Kyoung Ah Kim, Sung Hoon Kim, Dong Jun Kim, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim, Seok Jin Nam, Jung Hyun Yang, Howe Jung Ree
- J Korean Endocr Soc. 1999;14(1):53-62. Published online January 1, 2001
- 1,069 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of ret/PTC rearrangement in papillary thyroid carcinomas has been found to have wide variance in different populations. Recent studies, however, have been reporting no significant geographical difference between Asian and Western countries. In addition, there are some arguments about the correlation of ret/PTC expression with clinical aggressiveness. We have performed this study in order to examine the prevalence of ret/PTC-1, -2 and -3 rearrangements in korean papillary throid carcinomas and to ascertain its clinical relevance. METHODS: Fourteen thyroid tumors histologically confirmed to be papillary carcinomas were included in this study. To find rearrangements, we adopted RT-PCR and automated direct sequencing. Initial and follow-up clinical data were obtained form the patients medical records. The plasmid containing ret/PTC-2, and 3 was kindly provided by Dr. Ahn (Ulsan University, Seoul Choonang Hospital). RESULTS: We identified one tumors containing ret/PTC-1(1/14, 7.1%), and two containing ret/PTC-2 (2/14, 14.2%), and could not find ret/PTC-3 rearrangement in other patients (0/11). There was no significant correlation of ret/PTC with clinical aggressiveness. CONCLUSION: We found that the prevalence of ret/PTC rearrangement (3/14, 21.4%) in papillary thyroid carcinomas from Korea was similar to those recently reported in other nations. ret/PTC rearrangement may not affect biological behaviors of papillary thyroid carcinomas.


 KES
KES

 First
First Prev
Prev



